aHUS
(atypical Haemolytic Uremic Syndrome)
About aHUS
Atypical Haemolytic Uremic Syndrome (aHUS) is a systemic, progressive and potentially fatal disease.
It is caused by chronic, uncontrolled complement activation that leads to thrombotic microangiopathy (TMA) and severe terminal organ damage.1,2
The disease
aHUS is the result of a mutation in one or more complement-regulating genes, which leads to uncontrolled, excessive complement activation.4,5,6
In healthy individuals, complement works to defend against foreign particles and the system is regulated perfectly in order to prevent damage to organs and tissue. However, in patients with aHUS, the underlying gene mutations mean the complement cannot be controlled when it is activated.4
aHUS (atypical Haemolytic Uremic Syndrome) is caused by chronic, uncontrolled activation of complement, which is part of the body's immune system. This causes complement-mediated thrombotic microangiopathy (TMA), which is the formation of clots in small blood vessels throughout the body.1-4 TMA can lead to strokes, heart attacks, kidney failure and premature death.
aHUS KDIGO
Watch this video to learn about the conclusions published by the Kidney Disease Improving Global Outcomes (KDIGO) organisation, including the diagnostic flowchart for thrombotic microangiopathy or TMA, and the best treatment options for these conditions.
aHUS and pregnancy
The video discusses the significant risk of thrombotic microangiopathies (including thrombotic thrombocytopenic purpura and haemolytic uremic syndrome) during pregnancy and childbirth.
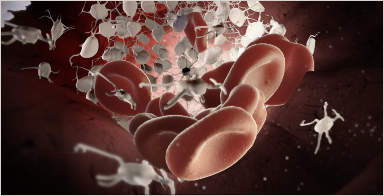
TMA and aHUS
This video explains the differential diagnosis of TMA.3

aHUS and kidney transplantation
This explains why an aHUS diagnosis is often associated with transplantations – a major risk factor for end-stage renal disease or death.1
Diagnosis
Conditions in which TMA occurs include Shiga toxin-induced haemolytic uremic syndrome (STEC-HUS), thrombotic thrombocytopenic purpura (TTP) and atypical haemolytic uremic syndrome (aHUS).1,7 aHUS is a rare, progressive and potentially fatal disease caused by chronic, uncontrolled activation of the alternative complement pathway.4,5 If left untreated, patients with aHUS are at risk for end-stage renal disease (ESRD), failures of other organs and premature death.4,6,8
Thrombotic microangiopathies (TMA) are a group of diseases characterised by thrombocytopenia, microangiopathic haemolytic anaemia and organ dysfunction. Ischaemic damage can occur in the brain, kidneys, heart, pancreas and lungs, among others.1,9 TMAs exhibit similar signs and symptoms, but are due to other causes.1,7
