About PNH
Paroxysmal Nocturnal Haemoglobinuria (PNH) is a rare and potentially fatal condition characterised by complement-mediated haemolysis.1,2
In cases of PNH, red blood cells are therefore highly susceptible to terminal complement-mediated intravascular haemolysis.1
PNH is a systemic disease with multi-organ involvement. The most common complication in PNH is venous thrombosis, which usually occurs in unusual locations and is the leading cause of death.
1,3,4
Although larger clone sizes have been associated with an increased risk of TE, all patients with PNH were at risk of TE regardless of clone
size.5


Signs and symptoms
In PNH, patients suffer from a spectrum of symptoms that vary from person to person:
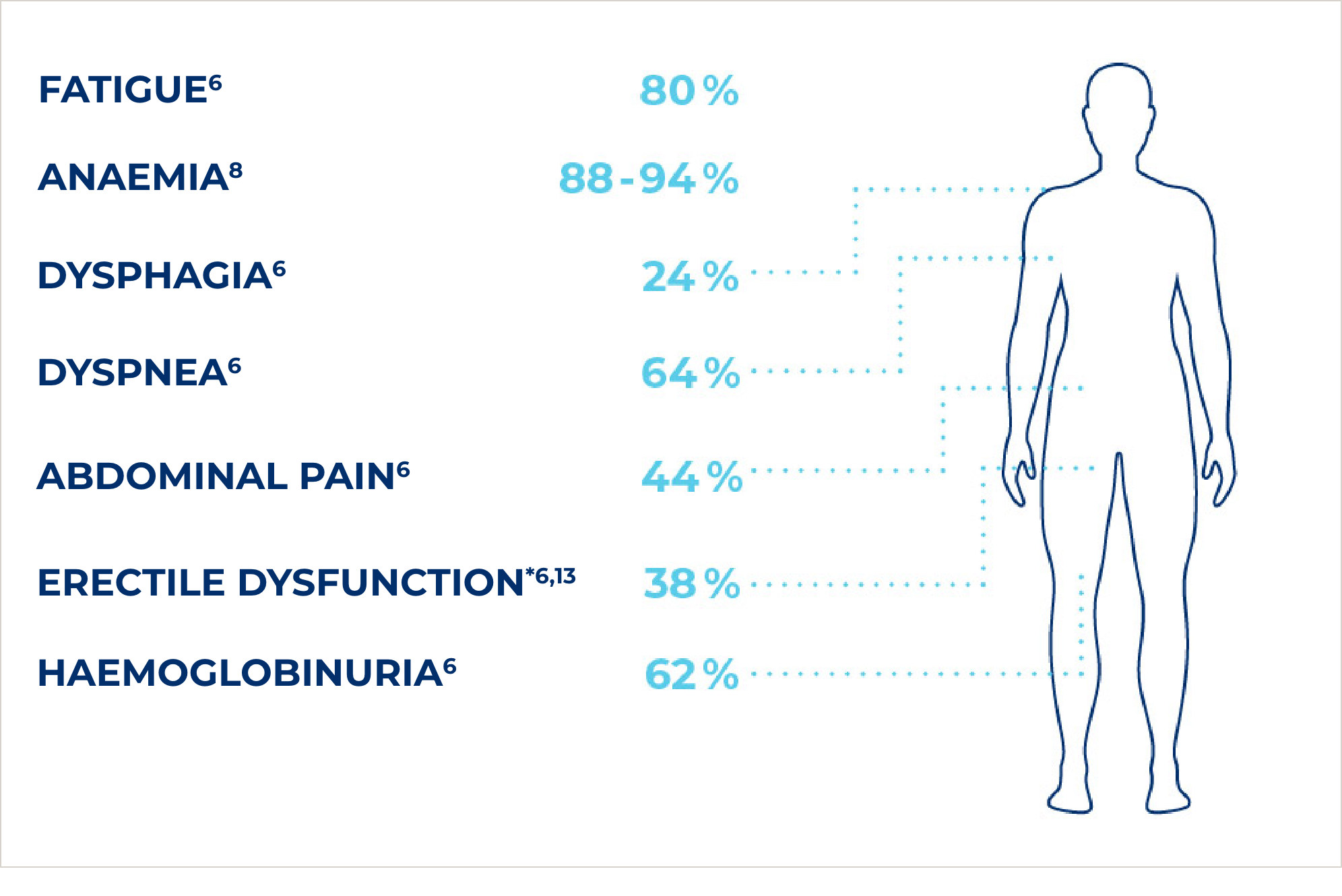
*male patients only (n=410)14
Symptoms
The most common symptoms and signs of PNH are anaemia, fatigue, dyspnoea, dysphagia, abdominal and chest pain and erectile dysfunction. The combination of one or more of these symptoms in conjunction with an LDH level greater than or equal to 1.5 times the upper limit value (ULN) is referred to as high disease activity (HDA).3,4,6
These symptoms can be debilitating and significantly reduce the quality of life of patients with PNH.5,6
The presence of haemolysis (elevated LDH) in association with clinical symptoms is associated with an increased risk of thrombotic events (TE).1 Pulmonary hypertension and renal failure are also complications of PNH.1,4,8
In addition, the association with bone marrow failure - especially aplastic anaemia9,10 - has been widely documented. Much less commonly, PNH may be associated with myelodysplastic syndromes (MDS), particularly refractory anaemia.11
Therefore, early diagnosis and regular determination of LDH levels and monitoring for signs and symptoms of High Disease Activity (HDA) is important.7
Diagnosis
The diagnosis of PNH (Paroxysmal Nocturnal Haemoglobinuria) is based on clinical features and the presence of haemolytic anaemia (increased reticulocytes, increased lactate dehydrogenase and bilirubin, and decreased haptoglobin, accompanied by iron deficiency due to haemosiderinuria), particularly because it is associated with thrombosis and/or cytopenia in the peripheral blood.2,12
Flow cytometry is used for diagnosis to detect a deficiency of GPI-linked antigens (CD44 and CD59) on red blood cells, monocytes and granulocytes and to determine clone size (percentage of abnormal cells).2,12
